Send. Track. Prove.
Rota Health automates the manual workflow of provider roster reconciliation by automatically handling updates across payers, continuously monitoring directories, and identifying discrepancies before they cause denials.
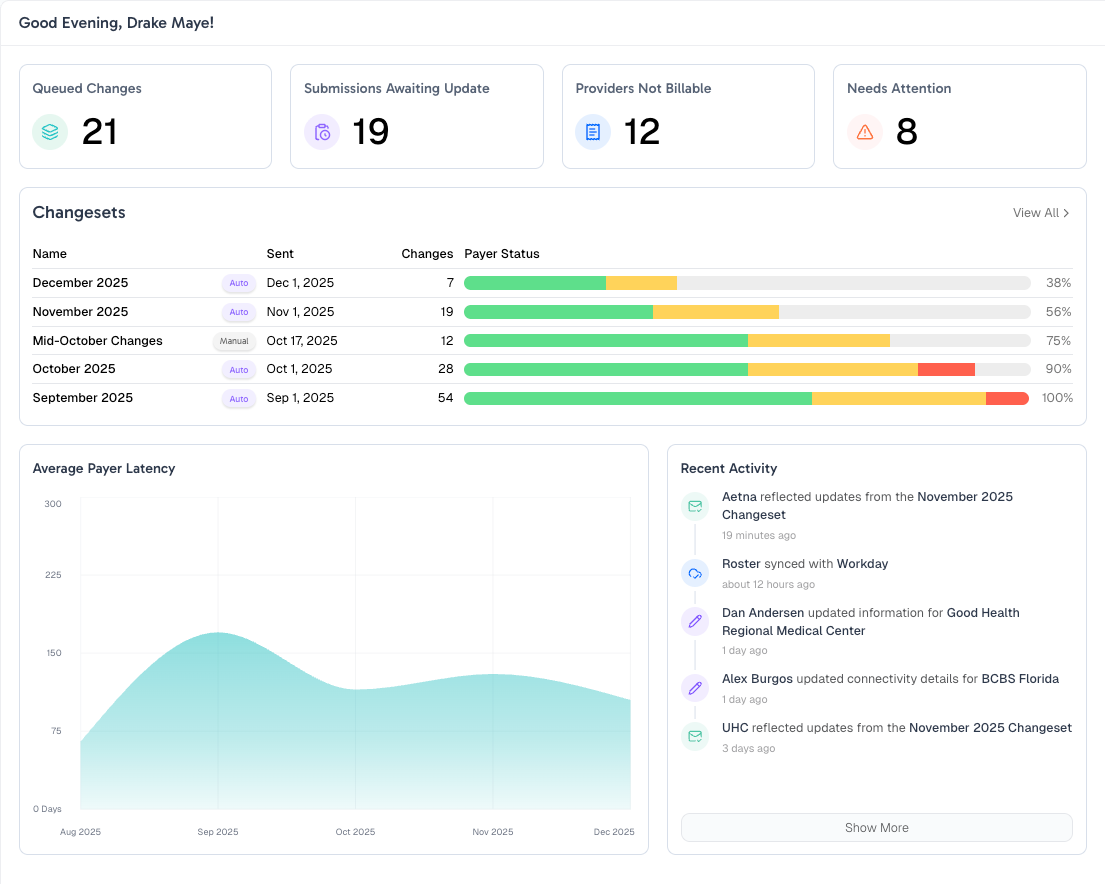
One dashboard. Every payer.
Track what's queued, what's waiting on payers, who can't bill yet, and what needs attention.
All in one place.
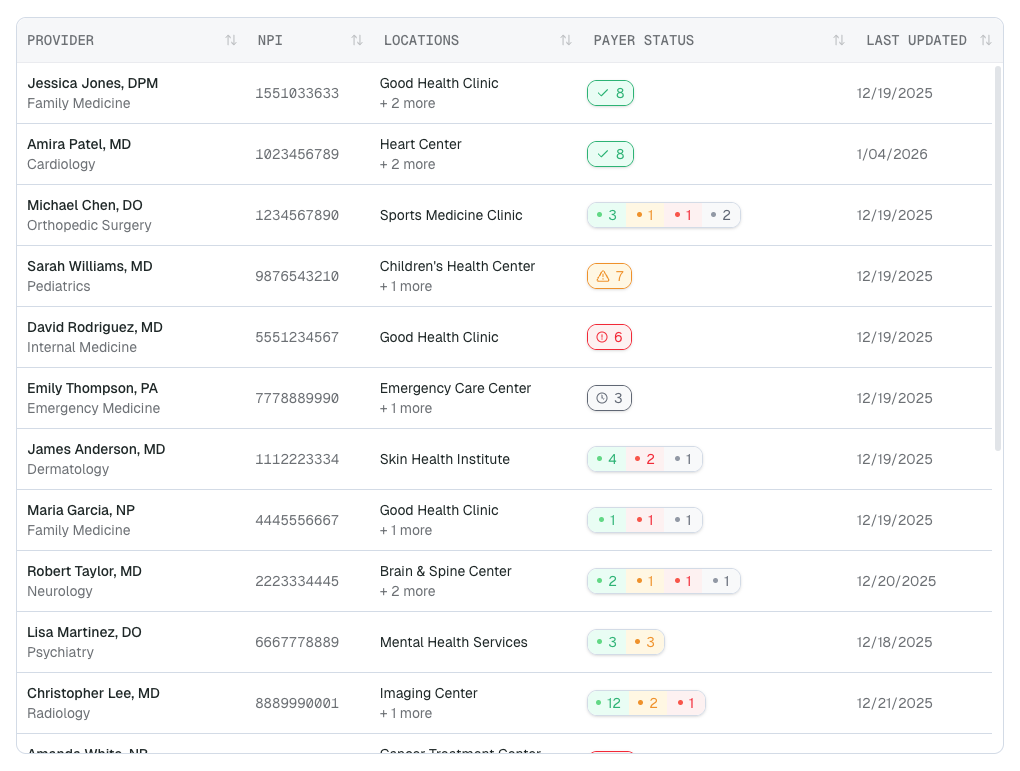
Directory updates, delivered instantly.
No more logging into portals one by one. We monitor every payer continuously. The moment your provider is reflected, you'll know.
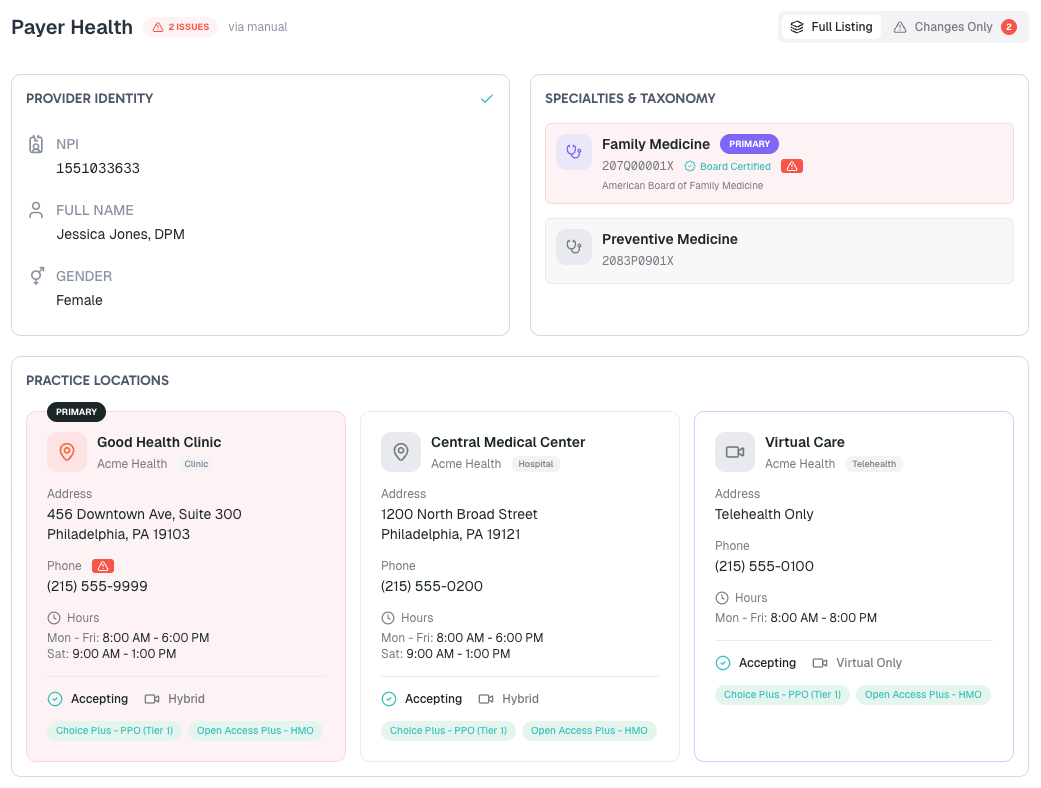
Early detection, fewer rejections.
A single identity, taxonomy, or location mismatch can kick back months of claims. See exactly what each payer has on file, field by field.
Built for teams buried in roster work.
Credentialing Teams
Stop chasing payer portals. Know exactly where every provider stands.
Revenue Cycle Leaders
Fewer denials from stale directory data. Faster time to bill.
Provider Operations
Manage thousands of providers across dozens of payers without the chaos.
We're working with a small group of design partners to get this right. If roster management is eating your time, we'd love to hear from you.